Contact Us
CiiS Lab
Johns Hopkins University
112 Hackerman Hall
3400 N. Charles Street
Baltimore, MD 21218
Directions
Lab Director
Russell Taylor
127 Hackerman Hall
rht@jhu.edu
Last updated: 2/28/19 and 9:09PM
The goal of this project is to evaluate the current AR-Guided Ventriculostomy System, improve upon the guide line visualization, and to create a training module for the catheter insertion using this system that provides additional multi-modal feedback.
 Ghandorh, Hamza & Mackenzie, Justin & De Ribaupierre, Sandrine & Eagleson, Roy. (2017). Development of Augmented Reality Training Simulator Systems for Neurosurgery Using Model-Driven Software Engineering.
Ghandorh, Hamza & Mackenzie, Justin & De Ribaupierre, Sandrine & Eagleson, Roy. (2017). Development of Augmented Reality Training Simulator Systems for Neurosurgery Using Model-Driven Software Engineering.
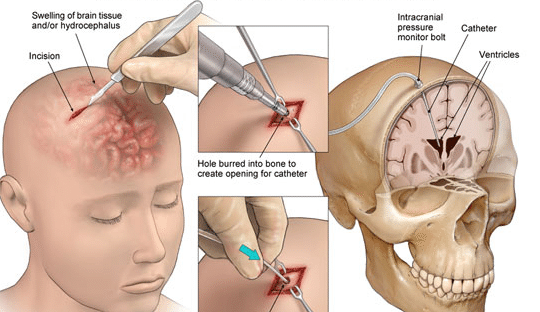
A ventriculostomy is a procedure conducted by neurosurgeons bedside to relieve pressure in the brain. This procedure is done by drilling a burr hole and inserting a catheter into a ventricle to drain cerebrospinal fluid. The target of this procedure is the Foramen of Monro. Surgeons largely rely on spatial temporal reasoning, because they look at a CT scan to guide this procedure, and experience. In addition, because patients have various anatomies, the Foramen can be shifted. This results in misses in about a third of insertion attempts. That’s not ideal because generally this procedure is time sensitive as pressure in the brain continues to build during failed attempts.
There already has been a HMD system created, by my mentors on this project, which provides a voice-activated navigational system that overlays the target ventricle on the patient’s head and also a planned path of catheter insertion customizable by the user. This system uses Hololens to project all of the visualization.
To test this system, a phantom was created. The phantom has registration fiducials on the front of the skull, a sample burr hole on the top of the head, and openings on the side for horoscope cameras to look in. Inside the plastic skull is the “brain of the phantom. The “brain” is made out of gelatin and there are three balls embedded in it, where are the possible shifts/locations of the foramen. These balls are the sample targets for this procedure. In order to use this phantom, a CT scan has been taken and then doctored so that the foramen is at each one of those balls.
The overall workflow of this current system is calculating the wearer’s interpupillary distance (provided by Hololens), register the CT scan to the patient’s head, and then plan the path at which the surgeon would insert the catheter along.
Hypothesis: AR-Guided ventriculostomy increases accuracy, efficiency, and decreases mental task load.
The users will be neurosurgery residents of varying expertise. It is a within-subject study meaning that they will be doing catheter insertions with and without the AR system. For each condition, there will be three targets (aka three trials). Data will be recorded through video of the attempts and a questionnaire. The questionnaire would contain such measurements as the System Usability Scale (SUS), Demographics, and NASA Task Load Index. SUS is a well established 10 question scale determine how usable the system is. Demographics are important because experience, as mentioned above, is an important factor in the success of this procedure. NASA TLX is another well established scale used to measure mental load of the workflow. See Project Files for the introductory tutorial video used for the user study.
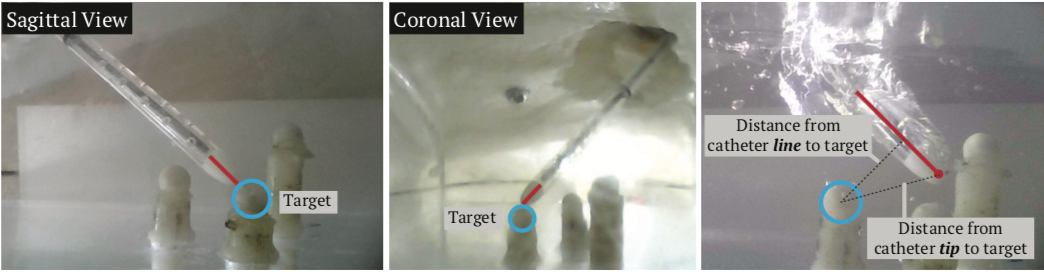 Task accuracy will be determined by two borescope cameras implanted in the skull. These cameras have an average error of 0.3mm. There were two measures for task accuracy: distance between catheter tip and target and the distance between catheter line and target, meaning the closest distance between the catheter and target. The reason we have the second measure is that the HMD system does not provide any guidance of how far to stick the catheter in. The users just needed to know that they have to insert it in 6cm. So, during the user study, users would insert the catheter hit the target and keep inserting past it. The reason that we felt this is a valid measurement is that, in the actual procedure, if the catheter hits near the target (within ~3mm), liquid would come out.
Task accuracy will be determined by two borescope cameras implanted in the skull. These cameras have an average error of 0.3mm. There were two measures for task accuracy: distance between catheter tip and target and the distance between catheter line and target, meaning the closest distance between the catheter and target. The reason we have the second measure is that the HMD system does not provide any guidance of how far to stick the catheter in. The users just needed to know that they have to insert it in 6cm. So, during the user study, users would insert the catheter hit the target and keep inserting past it. The reason that we felt this is a valid measurement is that, in the actual procedure, if the catheter hits near the target (within ~3mm), liquid would come out.
Participants: Ten participants were recruited for this user study. The participants' ages ranged from 21 to 35 (M = 25.44, SD = 5.11). All had an engineering or medical background. Participants reported that they were somewhat familiar with the mixed reality devices (M = 2.7, SD = 0.82) on a 5-point scale, with 5 being very familiar. The majority of participants had never viewed the ventriculostomy procedure. We did, however, have one neurosurgeon, who is experienced in this procedure, as part of the study. All participants were unpaid volunteers.
We used one-way ANOVA to determine the statistical significance between two groups where the fixed effect was with or without AR and the random effect was the participants.
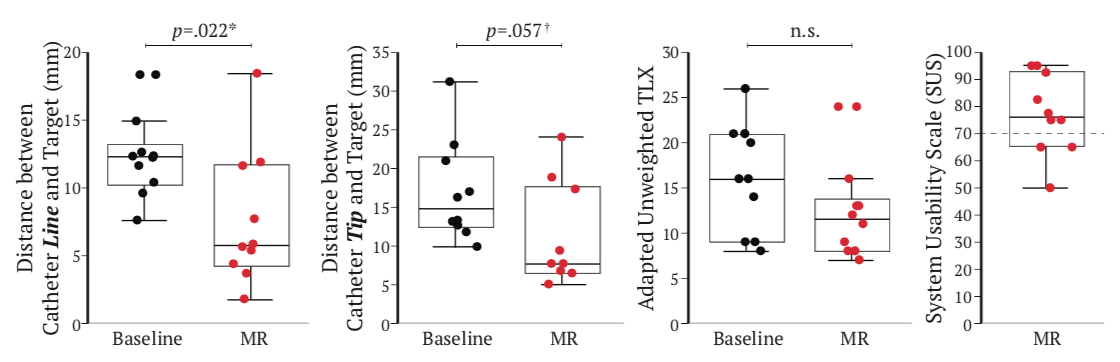 Task Accuracy: For distance between the catheter line and target, there was significant measured difference, F (1, 18) = 6.24, p = .022, between the two conditions. The participants with the mixed reality aid were able to maintain a shorter distance to the target (M = 7.63, SD = 5.00) when compared to using the baseline setup (M = 12.21, SD = 2.93). The measure for the distance between the catheter tip and target showed that there was a marginal improvement, F(1, 18) = 4.14, p = 0.057, in accuracy from non-assisted to assisted. Using mixed reality, participants were able to achieve an average accuracy of 10.96mm (SD = 6.61) and without was 16.93mm (SD = 6.52).
Task Accuracy: For distance between the catheter line and target, there was significant measured difference, F (1, 18) = 6.24, p = .022, between the two conditions. The participants with the mixed reality aid were able to maintain a shorter distance to the target (M = 7.63, SD = 5.00) when compared to using the baseline setup (M = 12.21, SD = 2.93). The measure for the distance between the catheter tip and target showed that there was a marginal improvement, F(1, 18) = 4.14, p = 0.057, in accuracy from non-assisted to assisted. Using mixed reality, participants were able to achieve an average accuracy of 10.96mm (SD = 6.61) and without was 16.93mm (SD = 6.52).
Mental Workload: The mental workload for executing a mock ventriculostomy procedure with and without AR was determined through a NASA TLX questionnaire. It turns out there was no statistically significant difference, F(1, 18) = 2.44, p = 0.136 between mixed reality (M = 12.01, SD = 5.04) and without (M = 16.00, SD = 6.07). However, it did seem that the mixed reality required less mental workload than without.
Usability: Participants fill out the SUS questionnaire that assesses how useable they thought the system was. The average for the system was 77.25 (SD = 14.69) and this is a well-established scale that suggests systems to have a score of at least 70 to be considered usable.
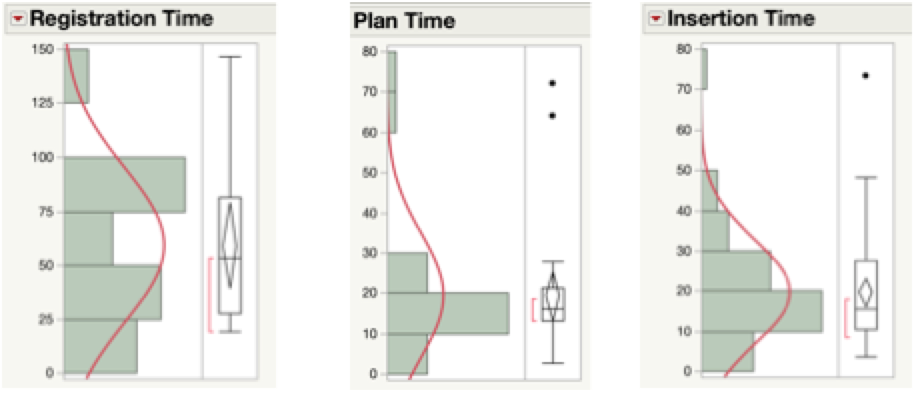 Additional Time Needed: This measure, as mentioned above, was broken down into three parts (see Figure 6). For the registration step, between the Hololens and the phantom, the average time for registration was 52 seconds (SD = 35.39) and for the neurosurgeon was about 18.99 s. The second step was the planning part of the workflow. The average time was 19.44 s (SD = 15.35) and the neurosurgeon’s time was 10.14s. Then for the insertion times for both conditions (baseline and with AR), the average time was 19.67s (SD = 12.93) and the surgeon’s was 11.72 s.
Additional Time Needed: This measure, as mentioned above, was broken down into three parts (see Figure 6). For the registration step, between the Hololens and the phantom, the average time for registration was 52 seconds (SD = 35.39) and for the neurosurgeon was about 18.99 s. The second step was the planning part of the workflow. The average time was 19.44 s (SD = 15.35) and the neurosurgeon’s time was 10.14s. Then for the insertion times for both conditions (baseline and with AR), the average time was 19.67s (SD = 12.93) and the surgeon’s was 11.72 s.
If the insertion times were are separated by condition (see Figure 7), there is a noticeable difference, U = -1.76, p = 0.79, r = - 0.33, between the baseline (Mdn = 12.50), which is slightly faster, and the AR system (Mdn = 18.07). This difference was also reflected in the neurosurgeon’s averages: baseline was 10.44s (SD = 3.38) and AR was 13.44s (SD = 2.75). AR insertion times were expected to take longer as the participants have to spend time trying to line the catheter up with the projected guideline. It is important to note that there does not seem to be any correlation between insertion time and accuracy, r(51) = -0.01, p = 0.89. This is the same case when the insertion times are separated by condition: baseline was r(24) = 0.063, p = 0.77 and r(24) = -0.059, p = 0.77.
Re-registration Frequency: Participants need to re-register the Hololens on average 1.67 times (SD = 1.12) with the averages per fiducial (3 fiducials) being around 2 times, shown in Figure 8. The general reasons for why the HMD needed to be re-registered were that the registration was done poorly in the first place: this was the first time for most participants using this system, and over time registration can shift. It is important to note that, for the person who had to re-register the system 4 times, this was due to the Hololens having to re-start. The neurosurgeon did not have to re-register at all.
Here give list of other project files (e.g., source code) associated with the project. If these are online give a link to an appropriate external repository or to uploaded media files under this name space (456-2020-11).
The tutorial video used in the user study is linked here: Tutorial Video
Part of the work above has been submitted in a MICCAI 2020 paper, An Interactive Mixed Reality Platform for Bedside Surgical Procedures. The other authors for this paper are: Ehsan Azimi, Zhiyuan Niu, Ruby Liu, Nicholas Greene, Camilo Molina, Judy Huang, Chien-Ming Huang, Peter Kazanzides.