Table of Contents
TEP Insufflator
Summary
TEP Insufflation device that improves the lives of those who have undergone tracheotomy
- Students: Rahul Modi
- Mentor(s): Dr. Jeremy Richmon
Background, Specific Aims, and Significance
Background:
In the United States, approximately 3,000 patients undergo laryngectomy on a yearly basis. Since the larynx (aka voice box) is generally removed in this procedure, the patient is unable to speak without assistance. This process, known as tracheo-esophageal speech, allows the patient to cover his/her stoma (the hole in the neck) to produce sound, which turns into understandable speech based on the mouths and tongues movements. We propose a modified CPAP device to insufflate a patient’s TEP, via a small caliber tube, to allow fluent tracheo-esophageal speech without the need to manually occlude the stoma.
Specific Aims:
- Eliminate the effort required in covering the stoma by introducing a constant air flow
- Devise a method to allow the patient to enable/disable the ability so speak without using his/her thumb or fingers
- Overall, eliminate the social stigma, discomfort, and fatigue that patients undergo when using their hand to cover their stoma
Significance:
- As many patients suffer from tracheo-esophageal punctures, this project aims to eliminate key issues that patients face in their day-to-day lives
Deliverables
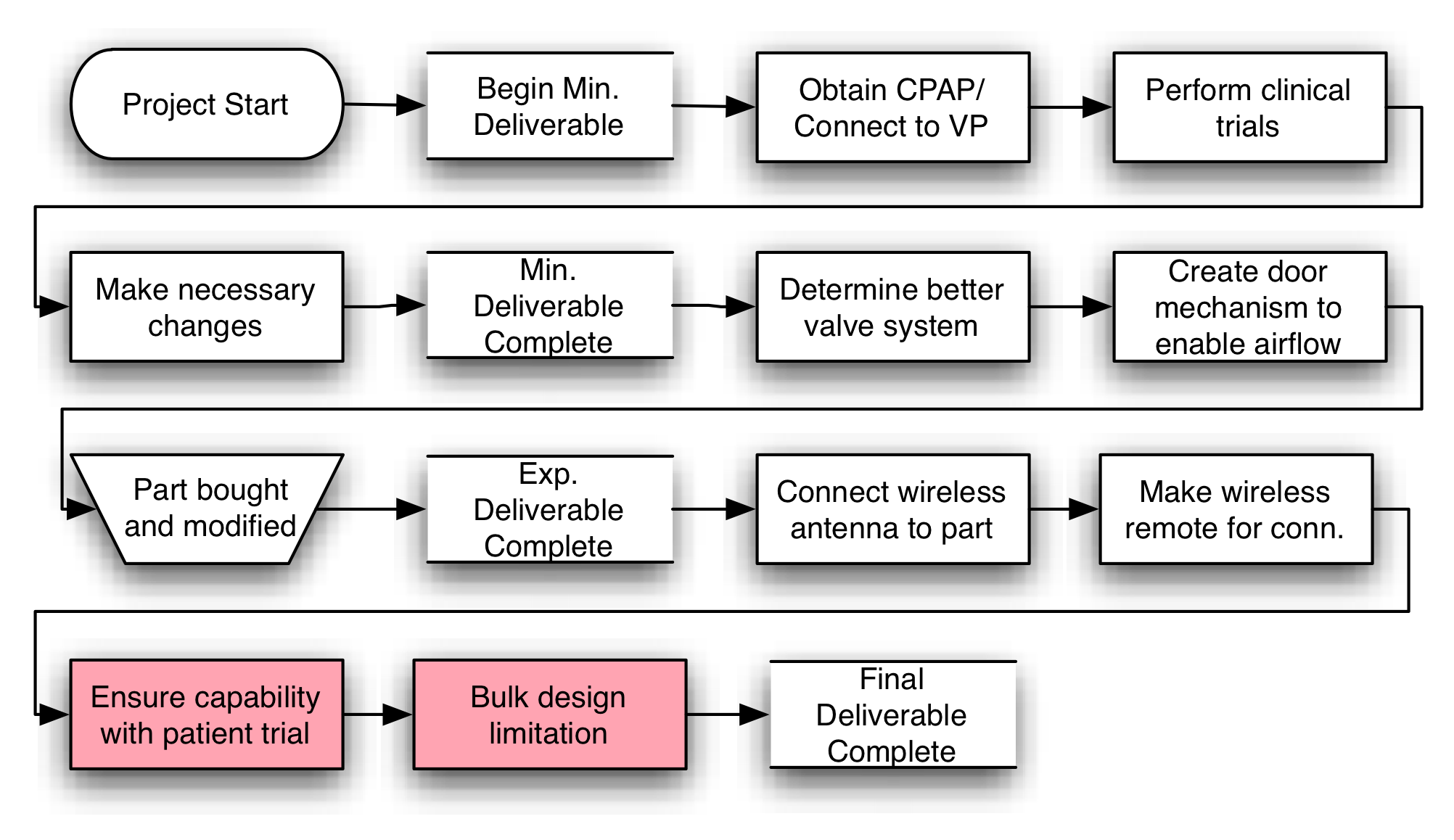
- Minimum: (Accomplished)
- Create a method of connecting a given CPAP machine to the voice prosthesis. Make sure that the connection is snug, but removable, between the devices
- Expected: (Accomplished)
- Create a finger-valve on the tube of the CPAP machine to allow patients to enable/disable the air flow from the machine
- Maximum: (Abandoned)
Technical Approach
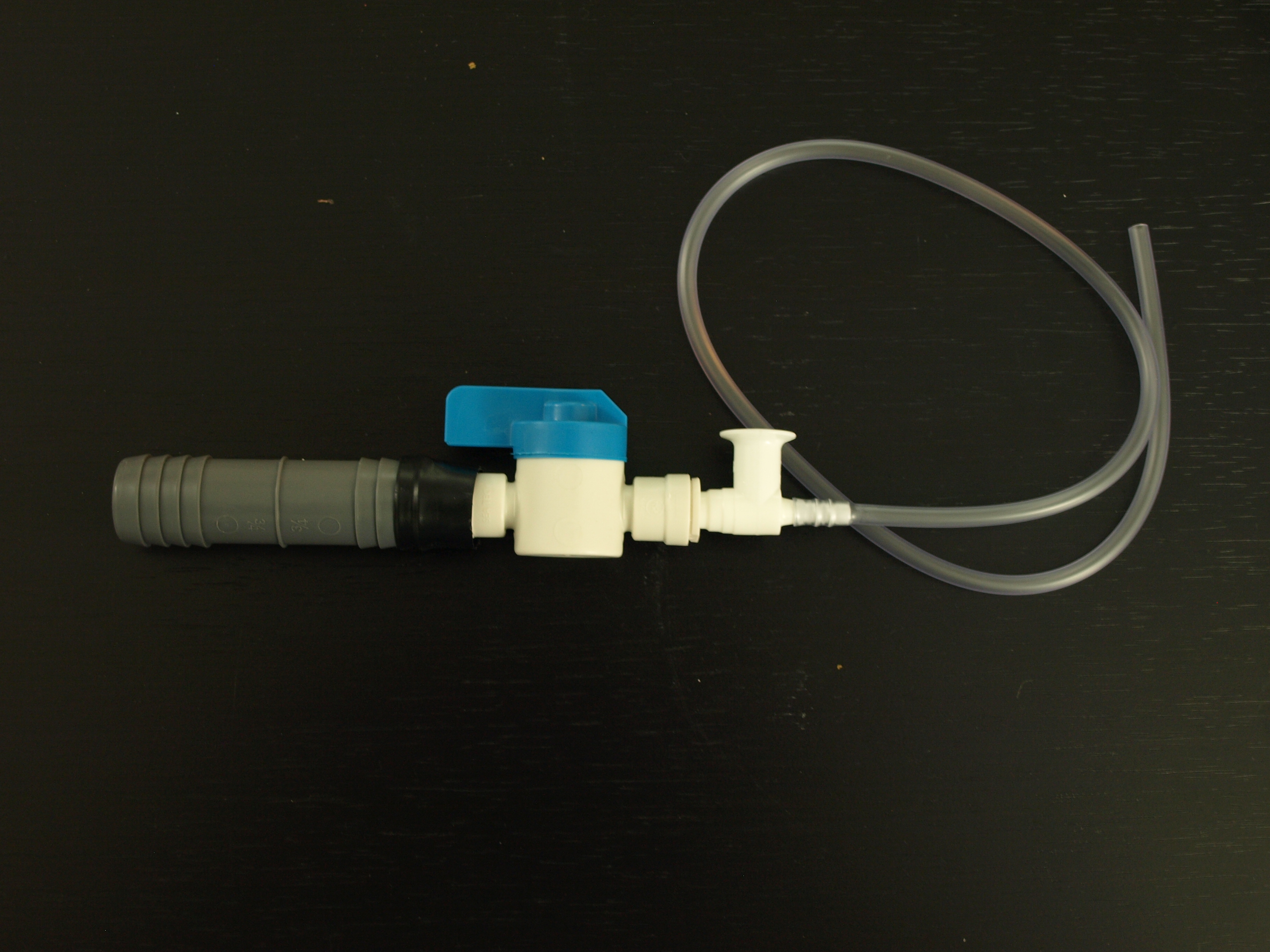
The overall goal of the TEP Insufflator is to provide patients who have undergone total laryngectomy with a simple, versatile, solution affiliated with speech. As explained in the background section, the current solution involves a manual closure of the patient’s stoma. In order to successfully eliminate the manual need to close the stoma, we will be connecting the voice prosthesis to a CPAP device. The CPAP device is used to provide a constant flow of air. When the CPAP device is turned on, it produces a constant flow of air to the patient’s TEP. This airflow blows through the insufflator into the patient’s TEP and allows him/her to generate sound in a way similar to that of occluding the stoma manually. As CPAP devices take time to turn on and off, a finger-valve was developed to allow the patient to quickly enable and disable airflow. With a simple turn, the patient is able to turn airflow on to occlude the TEP and generate voice.
The finger-valve used in the insufflator is an easy to use, rotating valve that features a circular wall within the valve. Specifically, when the cap of the valve is rotated 90º, the valve opens, allowing the air to go through. Likewise, when the cap is turned back to its original position, the valve closes, preventing all air from passing. This allows the patient to quickly and easily enable/disable airflow. This works under the assumption that the CPAP device is turned on and left at this position. Turning the CPAP on and off every time is unpractical and time consuming. Moreover, if the patient tries to speak while the device is powering on/off, he/she will belch.
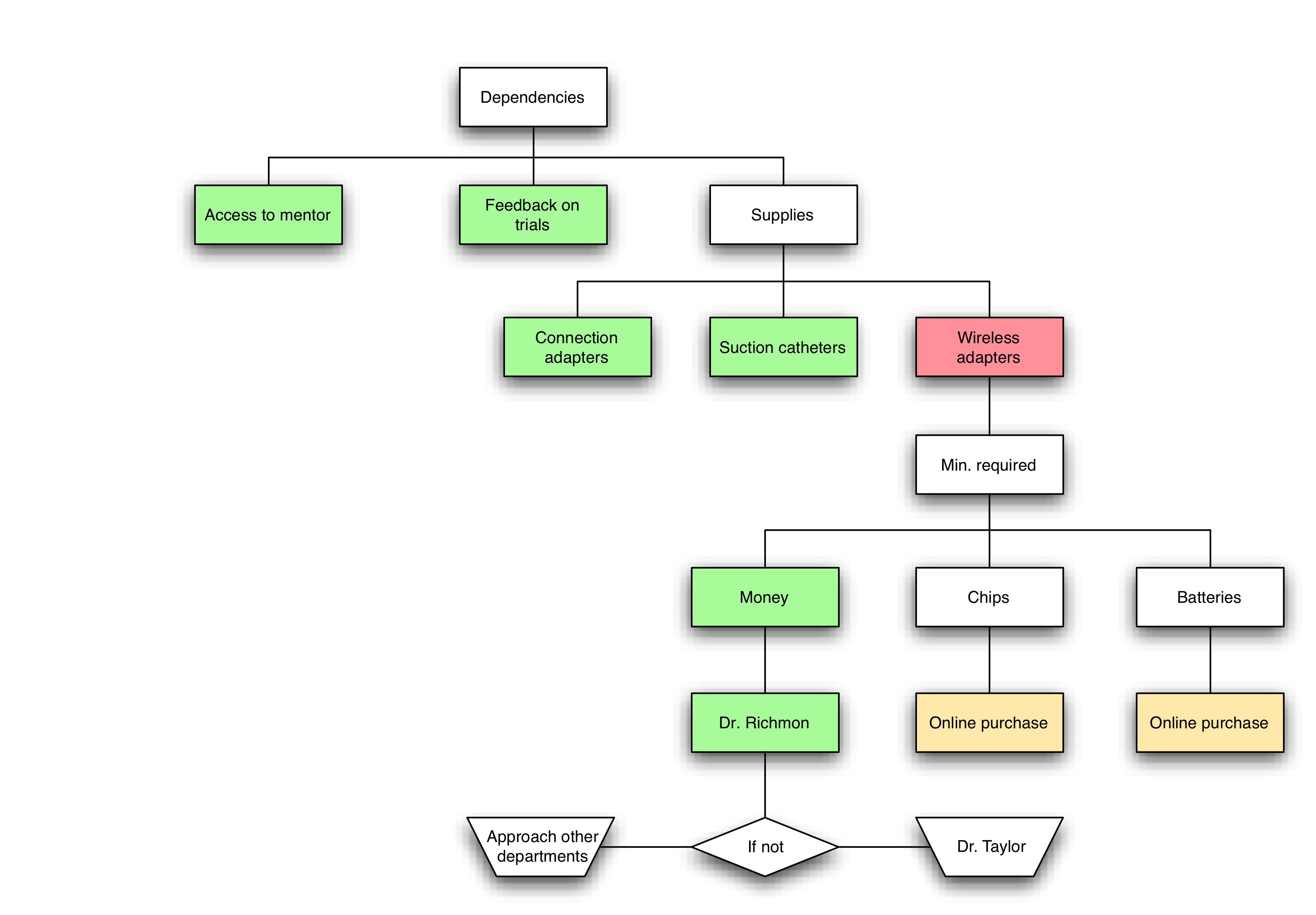
Dependencies
A block diagram of the dependencies can be found in the attachment. As shown in the diagram, the only limiting dependency including funding for the parts necessary to complete this project. Recently, my mentor informed me that funding for the parts will be provided by him; hence, there are currently no limiting dependencies.
Milestones and Status
- Milestone name: Minimum Deliverable
- Planned Date: None
- Expected Date: None
- Status: Completed
- Milestone name: Expected Deliverable
- Planned Date: April 1, 2014
- Expected Date: April 1, 2014
- Status: Completed
- Milestone name: Maximum Deliverable
- Planned Date: April 1
- Expected Date: None
- Status: Abandoned. Please see comments in Final Report to why maximum was not completed
Reports and presentations
- Project Plan
- Project Background Reading
- See Bibliography in Project Plan Proposal.
- Project Checkpoint
- Paper Seminar Presentations
- Project Final Presentation
- Project Final Report
Project Bibliography
- Sievers, Walker, & Rafii. (n.d.). Laryngectomy. Retrieved February 15, 2014, from University of California Davis Health System: http://www.ucdmc.ucdavis.edu/otolaryngology/Health%20Information/LARYNGECTOMY.pdf
- Staff, M. C. (2012, September 13). Throat cancer. Retrieved January 10, 2014, from Mayo Clinic: http://www.mayoclinic.org/diseases-conditions/oral-and-throat-cancer/basics/definition/con-20042850
- Steady Health. (2011, September 26). Definition And Important Facts About Laryngectomy. Retrieved February 4, 2014, from SteadyHealth.com: http://ic.steadyhealth.com/definition_and_important_facts_about_laryngectomy.html
- Marcus, C. L., Ward, S. L. D., Mallory, G. B., Rosen, C. L., Beckerman, R. C., Weese-Mayer, D. E., Brouillette, R. T., Trang, H. T. & Brooks, L. J. (1995). Use of nasal continuous positive airway pressure as treatment of childhood obstructive sleep apnea. The Journal Of Pediatrics, 127 (1), pp. 88–94.